Introduction
Fascioliasis is a rare parasitic infection of the hepatobiliary system caused by Fasciola hepatica and Fasciola gigantica. Symptoms include abdominal pain in the right upper quadrant, obstructive jaundice, and cholangitis [1, 2]. Extrahepatic manifestations are rare and have been reported in the subcutaneous tissue, brain, lungs, epididymis, and colon [3-6]. When extrahepatic fascioliasis appears as a tumor in the colon, malignancy can be mimicked, making it difficult to diagnose preoperatively [5, 6]. Herein, we report a case of hepatic and extrahepatic fascioliasis mimicking colon cancer with hepatic metastasis, in the form of multiple masses in the transverse colon and liver.
Case Report
A 60-year-old man visited our hospital for the evaluation of malignancy. He had experienced vague abdominal pain for 20 days. Laboratory findings showed elevated C-reactive protein (34.97 mg/L), normal white blood cell count (9450/μL), and eosinophilia (3450/μL, 36.5%). Tumor markers of carbohydrate antigen (CA) 19-9 and carcinoembryonic antigen (CEA) levels were within the normal range (CA 19-9, 4.0 U/mL; CEA, 0.61 ng/mL).
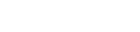
Abdominal computed tomography (CT) axial (Fig. 1A) and coronal (Fig. 1B) portal phase images showed irregular circumferential edematous wall thickening at the hepatic flexure of the colon. Extensive fat infiltration and edema were noted in the transverse mesocolon and greater omentum, and a small amount of ascites was observed. An axial CT portal image of the caudal side (Fig. 1C) showed multiple hypodense masses with an enhancing solid portion in the left hepatic lobe. The lesions were clustered in segment 3 and the fissure for the ligamentum teres. The initial diagnosis was mucinous colon cancer with microperforation and cystic hepatic metastasis. The differential diagnosis was severe colitis and hepatic abscess. On further evaluation using magnetic resonance imaging (MRI), the axial fat-suppressed T2 weighted image (Fig. 1D) showed circumferential T2 hyperintense wall thickening with a uniform layer of the transverse colon. Diffuse T2 hyperintense fat and perilesional fluid in the omentum and transverse mesocolon were noted, suggesting extensive edema and inflammation. Axial fat-suppressed T1 weighted image (Fig. 1E) showed a diffuse hyperintense signal of the omentum and transverse mesocolon, suggesting hemorrhage. Axial fat-suppressed T2 weighted image (Fig. 1F) showed multiple T2 bright hyperintense masses with internal intermediate signal intensity nodules in the left hepatic lobe. Tiny cystic lesions were observed along the fissure of the ligamentum teres. Linear elongated hyperintense foci along the periportal area and tram-track sign were observed. A tentative diagnosis from CT and MRI was parasitic infection with liver and colon involvement.
Colonoscopy (Fig. 1G) revealed a large infiltrative mass with ulceration and luminal obstruction, suggesting colon cancer. However, the biopsy result after pathological review revealed nonspecific inflammation. Positron emission tomography/computed tomography (PET/CT) imaging (Fig. 1H) revealed a high standardized uptake value (SUV) (maximum 6.9) in both colon and liver lesions, suggesting colon cancer with liver metastasis. Owing to the discordant workup results, a multidisciplinary approach was employed. Using ultrasound-guided aspiration of the liver lesion, a yellowish material was aspirated. A Fasciola hepatica eggs was detected. The serum Fasciola hepatica antibody test results were positive. After treatment with triclabendazole, the treatment of choice for fascioliasis, colon and liver lesions were improved by a follow-up abdominal CT scan (Fig. 1I, J).
Discussion
Fascioliasis is a zoonotic trematode infection caused by Fasciola hepatica and Fasciola gigantica, with Fasciola hepatica infection being the most common type of infection [7]. The endemic areas of human fascioliasis are South America, North Africa, and the Middle East, and cases are sporadically reported in Korea [2, 7, 8]. Freshwater snails are intermediate hosts, and mammals, including humans, are definitive hosts [1]. When encysted larvae from contaminated water are ingested by humans, the larvae penetrate the duodenal wall, enter the liver through the peritoneum and Glisson's capsule, and settle in the bile duct or gallbladder [1, 10].
The two stages in which the larvae infect the liver and cause symptoms are broadly divided into hepatic (acute) and biliary (chronic) [8, 9]. In the hepatic stage, the main symptoms are urticaria, abdominal pain, and fever, and in the biliary stage, intermittent abdominal pain and cholangitis or cholestasis are accompanied [9, 10]. Similarly, it is divided into the parenchymal and ductal phases in radiology [1]. In the parenchymal phase, multiple microabscesses are seen at the migration site of the larva, and a tunnel-like tract is seen at the entry site of Glisson's capsule [8, 10]. Upon penetration of the parenchyma, clustered abscesses appear as caves with a serpentine pattern. The 'tunnels and caves' sign observed on CT can be a characteristic sign of hepatic fascioliasis [9, 10]. In the ductal phase, at 8 weeks, a dilated biliary duct with portal tract thickening is observed. Calcifications of the subcapsular area can be observed after 10 weeks [1].
There have been reports of extrahepatic fascioliasis in the GI tract, including the colon, cecum, and transverse mesocolon [2, 5, 6, 11, 12]. Colon involvement is thought to be caused by the migration of penetrating larvae through the duodenal wall to a location other than the liver through the peritoneum or mesentery [1]. In this case, a mass in the proximal transverse colon was formed, accompanied by severe inflammation in the surrounding transverse mesocolon and greater omentum. CT showed increased fat density, fascial thickening, and perilesional fluid, and MRI showed T2 hyperintensity and bright high-signal intensity lesions, suggesting fluid collection and edema. One of the interesting points in this case was the T1 hyperintensity of the omentum and transverse mesocolon, suggesting hemorrhage. To the best of our knowledge, there are no reports of MRI findings of extrahepatic fascioliasis or T1 hyperintensity of the omentum and mesentery. However, there is a study reporting an MRI finding of T1 hyperintensity caused by larval penetration of the liver capsule, therefore we believe that the hyperintensity of peritoneal fat is likely due to the migration of the Fasciola larvae [1].
Even when only the liver lesion exists, malignancy such as cholangiocarcinoma can be mimicked [13], but it is relatively easy to diagnose hepatic fascioliasis through clinical symptoms, eosinophilia, and serum antibody [1, 8]. However, in this case, the diagnosis of colon cancer with hepatic metastasis was considered the initial differential CT diagnosis due to the simultaneous involvement of hepatic and extrahepatic fascioliasis, showing liver and colon lesions simultaneously. In particular, CT, endoscopy, and PET/CT showed diagnostic findings mimicking malignancy, such as colon mass with multiple liver masses, infiltrative colon mass with obstruction, and high F18-fluorodeoxyglucose uptake of those lesions, respectively. However, the MRI findings were helpful in the differential diagnosis. T2 bright high-signal intensity microabscesses in the liver parenchyma, ‘Tunnels and caves’ sign in the subcapsular and peribiliary areas, T2 hyperintense wall thickening with a uniform layered pattern of the colon, severe edematous changes, and hemorrhage of the omentum and transverse mesocolon helped diagnose hepatic and extrahepatic fascioliasis. In the previous case reports, there were cases in which colon cancer was mimicked, and surgical excision was performed [5, 6]. The combination of multimodality imaging helped diagnose the disease, and unnecessary surgical intervention was prevented in this case.
In conclusion, in cases of multiple cystic masses in the liver, a colon mass with poor enhancement, and severe inflammation in the surrounding omentum and mesentery, parasitic infection, specifically hepatic and extrahepatic fascioliasis, should be considered as the first diagnostic impression.


 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print






