경경정맥 간내 문맥 정맥 단락술 후 발생한 동맥-담관루에 의한 대량 혈담즙증 : 증례 보고
Massive Hemobilia Due to Arteriobiliary Fistula after the Transjugular Intrahepatic Portosystemic Shunt (TIPS): A Case Report
Article information
Abstract
경경정맥간내문맥정맥단락술은 조절되지 않는 불응성 복수, 흉수, 정맥류 출혈 치료에 효과적인 방법이지만 시술과 관련된 합병증 발생 위험이 높다. 혈담즙증으로 나타나는 동맥담관 누공은 경경정맥간내문맥정맥단락술의 주요한 치명적인 합병증 중 하나이다. 대부분의 경경정맥간내문맥정맥단락술관련 출혈은 주로 문맥 천자 과정에서 발생하는 합병증이다. 저자는 경경정맥간내문맥정맥단락술 시행 후 발생한 간동맥-담도 누공에 의해 발생한 대량 혈담즙증 1예를 보고하고자 한다.
Trans Abstract
The transjugular intrahepatic portosystemic shunt (TIPS) is an effective method for the treatment of uncontrolled refractory ascites, pleural effusion, and variceal bleeding, but the risk of complications related to the procedure is high. Arteriobiliary fistula, which is manifested as hemobilia, is one of the major fatal complications of the TIPS. Most of the TIPS-related bleeding is a complication that occurs mainly during the portal vein puncture. We are reporting a case of massive hemobilia due to hepatic arteriobiliary fistula caused by TIPS procedure.
Introduction
Although transjugular intrahepatic portosystemic shunt (TIPS) is an effective modality for treatment of uncontrolled refractory ascites, hydrothorax or variceal bleeding, the risk for procedure-related complications is high [1]. Arteriobiliary fistula presented by hemobilia is one of major fatal complications of TIPS [2]. Most TIPS associated bleeding is primarily a complication during puncture of portal vein [2]. We are reporting a case of massive hemobilia due to hepatic arteriobiliary fistula caused by TIPS procedure.
Case Report
A 47-year-old man with end-stage secondary to alcoholic liver disease was admitted to our hospital for uncontrolled massive ascites, and right hydrothorax. The transjugular intrahepatic portosystemic shunt (TIPS) was planned for refractory ascites and right pleural effusion. Initial hemoglobin and platelet were 8.3 g/dL (14−17 g/dL), and 105x103/ul (130−450x103/ul), respectively. Coagulation test data were as follows: PT, 1.36 (INR, 0.88−1.13); aPTT, 39.2sec (29.1−45.1sec). Laboratory tests data were as follows: total bilirubin, 5.6 mg/dL (0.2–1.2 mg/dL); direct bilirubin, 4.1 mg/dL (0.0–0.4 mg/dL); aspartate aminotransferase, 52 U/L (8–38 U/L); alanine aminotransferase, 16 U/L (5–43 U/L); alkaline phosphatase, 102 U/L (40–130 U/L); γ-glutamyl transferase, 188 U/L (11–75 U/L); protein, 6.1 g/dL (6.4−8.1 g/dL); albumin, 2.4 g/dL (3.8−5.3 g/dL). He had a successful TIPS procedure (mean portal-systemic gradient decreased from 41 mmHg to 20 mmHg). Seven days after the TIPS, he had hematochezia, hematemesis, tachycardia, hypotension, and worsening anemia (hemoglobin dropped from 8.3 g/dL to 3.0 g/dL in 4 hours). He was in circulatory shock and was transferred to the critical care unit. He underwent CT angiography for bleeding focus evaluation. On CT angiography, the TIPS stent was patent. However, the active contrast agent leakage was noted at the distal end of stent between the right hepatic artery and the right intrahepatic bile duct. The active contrast agent leakage progressed through the common bile duct and there was reflux into the gastric antrum and the duodenum (Fig. 1). The patient immediately underwent a percutaneous angiography. Celiac trunk arteriography revealed an active contrast extravasation into the common bile duct from the right hepatic artery via the arteriobiliary fistula (Fig. 2). Subsequently, selective embolization of right hepatic artery branches was successfully performed with coils, glue and gelatin sponge. However, the patient died one day after from the disseminated intravascular coagulation.
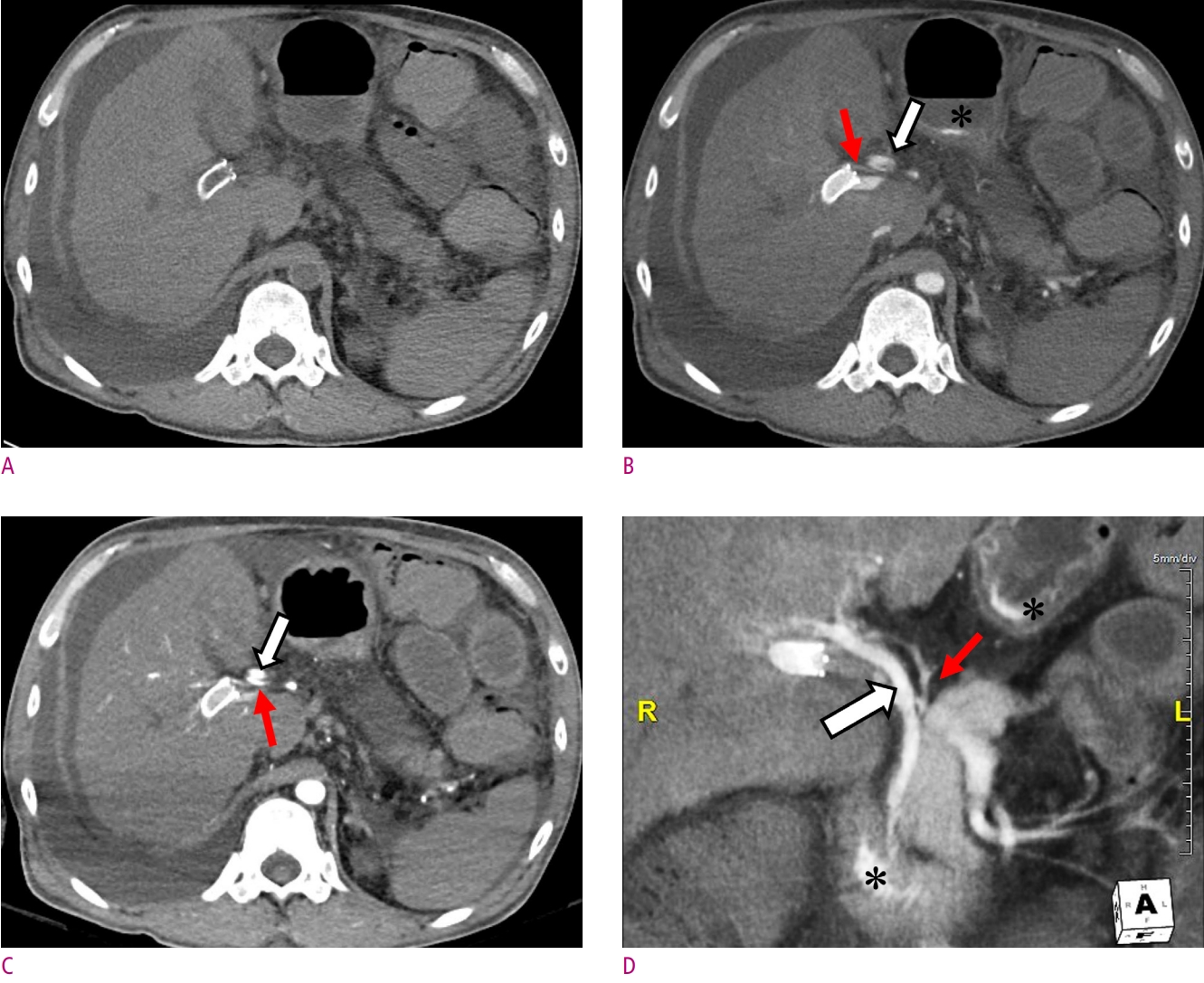
CT angiography of the arteriobiliary fistula in a 47-year-old male after TIPS.
(A) Precontrast axial CT scan shows the distal end of TIPS in right portal vein. Arterial-phase axial CT scan (B) shows right hepatic artery (red arrow), portal vein and TIPS stent filled with the contrast agent, and bile duct (thick white arrow). There is small amount of the contrast agent refluxed into the gastric antrum (*) from arteriobiliary fistula. Portal-phase axial CT scan (C) shows more dense enhancement of the right hepatic artery (red arrow) and the common hepatic duct (Thick arrow). Coronal reformatted multiplanar reconstruction image parallel to the common bile duct (D) shows an arteriobiliary fistula with active contrast agent extravasation between the right hepatic artery (red arrow) and the common bile duct (thick white arrow). The leaked contrast agent was excreted into the duodenum and refluxed into the gastric antrum (*) through the common bile duct.

Celiac angiography of the arteriobiliary fistula in a 47-year-old male after TIPS.
Early to late arterial phases (A-C) of celiac angiography show an arteriobiliary fistula with active contrast extravasation between right hepatic artery (red arrow) and right intrahepatic bile duct. Venous phase of celiac angiography shows an excreted contrast agent into the common bile duct (thick arrow).
Discussion
The TIPS is the percutaneous creation of a channel between the hepatic vein and the portal vein that is used to manage complication of portal venous hypertension [3]. Indications for TIPS include management of variceal bleeding, refractory cirrhotic ascites, hepatorenal syndrome, Budd-Chiari syndrome, and refractory hepatic hydrothorax [1, 3, 4]. As elevated portal pressure is one of the major factors contributing to the pathogenesis of ascites and hepatic hydrothorax, TIPS is a highly effective treatment option for them [5, 6]. Multiple studies have been published assessing the effectiveness of TIPS in patients with refractory ascites and technical success was achieved in 93–100% of cases, with control of ascites achieved in 27–92% and complete resolution in up to 75% of cases [1]. TIPS should be considered as a treatment option for patients who require frequent paracentesis (generally >3 in a month). In addition, TIPS has been shown to resolve hepatic hydrothorax in 60–70% of patients [5, 6].
While the primary technical success rate of TIPS placement is high, complications can occur and can drastically alter patient prognosis. Potential complications of TIPS include acute liver failure, hepatic encephalopathy, hemorrhage, biliary injury, injury to surrounding organs, TIPS thrombosis, TIPS dysfunction, and TIPS migration [1].
Serious arteriobiliary fistula complication presented as a hemobilia can occasionally occur in the early postprocedural period following TIPS placement [7]. Given the proximity of bile duct radicals to the branches of the hepatic artery and portal vein, the incidence of concurrent injury to these structures and consequent fistula formation is not unexpected. Approximately 3.8% incidence of hepatic vascular abnormalities was found following percutaneous transhepatic cholangiography [7, 8]. The frequency of clinical hemobilia is reported up to 5% after TIPS. Often hemobilia is a self-limiting phenomenon and expectant observation is a commonly used option. Clinically significant hemobilia presents with biliary colic, jaundice, and gastrointestinal bleeding, which may range from occult to massive bleeding. The initial diagnosis can be made with endoscopy [9]. CT angiography is an accurate, cost-effective tool to assess hemobilia, hematemesis, or hematochezia and can show the precise location of bleeding, thereby directing further management. Angiography with embolization is the treatment of choice for most cases of hemobilia. The goals of therapy in cases of hemobilia are to stop the bleeding and to restore bile flow. Angiography is clearly the most efficacious method for controlling intrahepatic bleeding sources, with success rates above 95% [10].
In conclusion, massive hemobilia is rare, but one of the possible complications of TIPS. A liver parenchymal puncture during a TIPS procedure may damage vascular structures such as the hepatic artery, portal vein, as well as bile duct. In cases of gastrointestinal hemorrhage after TIPS procedure, the possibility of hemobilia due to arteriobiliary fistula should be considered.