담낭암으로 오인된 담낭의 염증성 근섬유모세포 종양: 증례보고
Inflammatory Myofibroblastic Tumor of Gallbladder Mimicking Gallbladder Cancer: A Case Report
Article information
Abstract
담낭의 원발성 염증성 근섬유모세포 종양은 극히 드문 양성질환이다. 임상 및 영상의학적 소견은 비특이적이며, 흔히 악성종양과 유사한 소견을 보여 오인될 수 있어 감별을 요한다. 본 증례 보고는 69세 여자 환자에서 담낭에 생긴 원발성 염증성 근섬유모세포 종양이 수술전 영상에서 담낭암으로 오인되어 수술을 시행하였던 증례이다.
Trans Abstract
A primary inflammatory myofibroblastic tumor (IMT) of gallbladder is an extremely rare. Clinical and radiologic features of IMTs are nonspecific and can mimic malignant neoplasm. Herein, we present a case of gallbladder IMT, which was initially suspected to be gallbladder cancer preoperatively.
Introduction
Inflammatory myofibroblastic tumor (IMT) is a rare type of mesenchymal neoplasm that can occur in various parts of the body. The most frequently involved organ in the abdomen is the liver, while the primary IMT of gallbladder is quite rare [1-3]. It can present diagnostic challenges due to its potential resemblance to malignant neoplasms such as gallbladder cancer. In this case report, we will describe the clinical, imaging, and histopathological features of a patient diagnosed with gallbladder IMT, initially suspected to be a gallbladder cancer preoperatively. The purpose of this report is to describe the imaging findings of IMT of gallbladder and emphasize the significance of an accurate diagnosis.
Case Report
A 69-year-old female was referred to our hospital for weight loss of 5 kg in 6 months and abdominal discomfort. Upon laboratory tests, there were no significant findings, and the CA19-9 level was within normal limits.
A subsequent contrast-enhanced abdominal CT scan revealed the presence of a 3.5 x 6.0 cm mass in the gallbladder (Fig. 1). On non-contrast scan (Fig. 1A), the mass did not show definite calcification. In axial arterial (Fig. 1B) and portal venous (Fig. 1C) phases, the mass showed strong heterogeneous enhancement. The coronal reformatted image (Fig. 1D) showed focal enhancing thickening of the base of the gallbladder wall, where the large mass attached (arrow). An enlarged lymph node was found at pericholecystic area, just below the cystic duct (Fig. 1E).
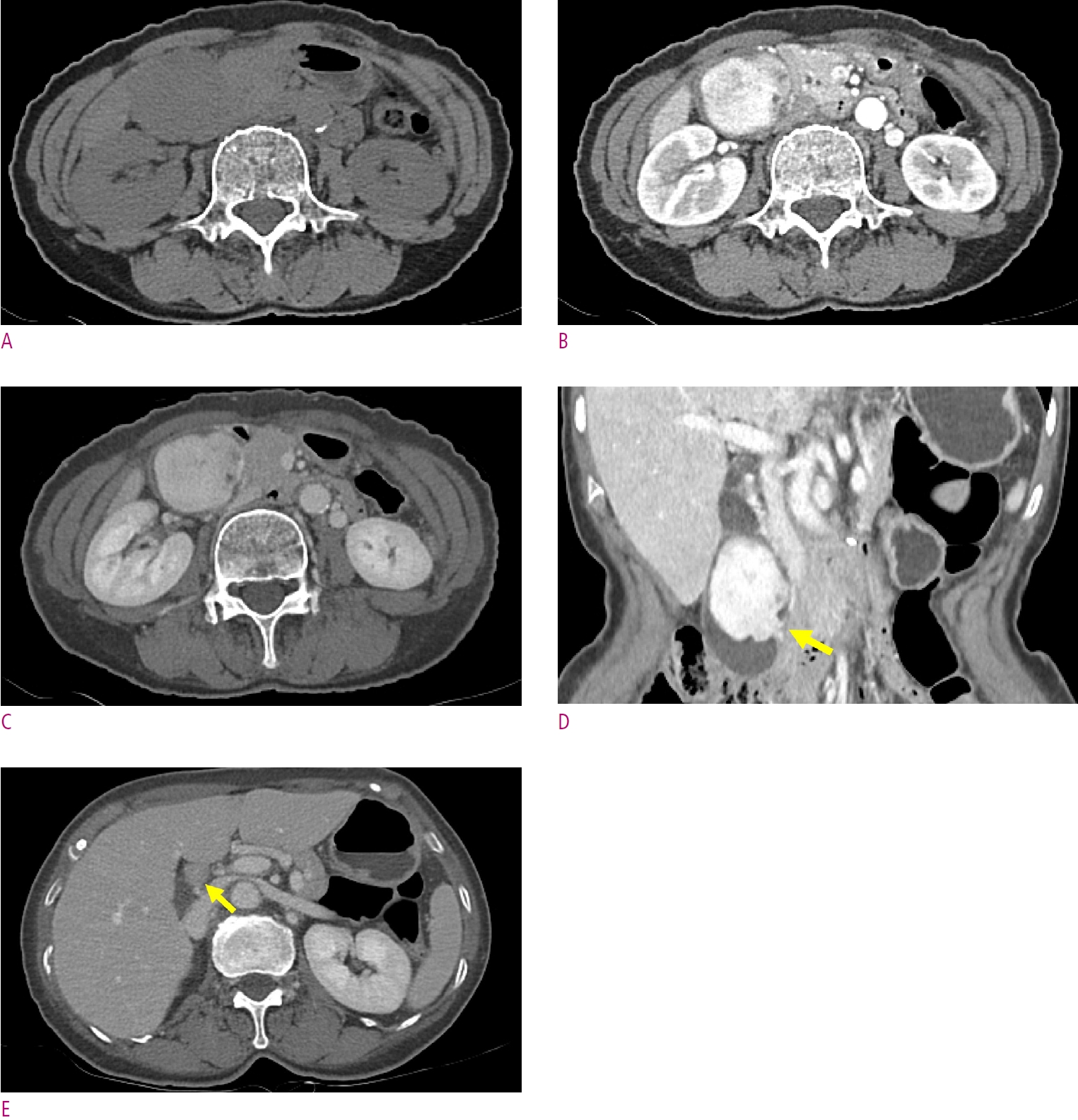
Multiphasic CT reveals a 3.5 cm mass in the gallbladder. On non-contrast scan (A), the mass shows homogeneous attenuation with no calcification. Arterial (B) and portal venous (B) phases show well-defined, endophytic lobulated mass that enhances well and heterogeneously. An enlarged lymph node exists at pericholecystic area (arrow) on portal venous phase scan (E).
On axial T2-weighted image (Fig. 2A), the mass showed heterogeneously hyperintense T2 signal with small cystic components. Compared to precontrast T1-weighted image (Fig. 2B), on arterial (Fig. 2C), portal venous (Fig. 2D) and delayed (Fig. 2E) phases of dynamic enhancement study using extracellular gadolinium-based contrast media revealed a lobulated mass showing heterogeneous, well and persistent enhancement. The mass showed definite diffusion restriction except for cystic components (Fig. 2F and G). The lymph node on the CT scan appeared as it was before.

MR images show a lobulated mass of the gallbladder. Axial T2-weighted image (A) shows a heterogeneously hyperintense mass with cystic or necrotic components. Precontrast (B) and dynamic enhanced (C-E) T1-weighted images show heterogeneously well-enhancing mass of the gallbladder. MR images show a lobulated mass of the gallbladder. Diffusion restriction of the mass except in cystic or necrotic areas is noted at the b value of 800 s/mm2 (F) and the corresponding apparent diffusion coefficient map (G).
On following transabdominal ultrasonography, the gallbladder mass showed heterogenous echogenicity with increased vascularity on Doppler imaging (Fig. 3A and B).

Transabdominal ultrasonography reveals a mass that fills the gallbladder. The gallbladder mass showed heterogenous echogenicity with increased vascularity on Doppler imaging (Fig. 3 A and B).
As a differential diagnosis, we considered gallbladder cancer considering the incidence and staged it as cT2 based on the focal wall thickening at the base. Additionally, we mentioned the possibility of metastasis in the pericholecystic lymph node. We planned surgery with the impression of gallbladder cancer and decided to perform only laparoscopic cholecystectomy first with pericholecystic lymph node dissection and additional surgery if necessary. Histopathologic examination of the resected specimen revealed a 10.4 cm IMT (Fig. 4). In 6 months of follow-up imaging after operation, no recurrence or metastasis was found in abdomen.

Histopathological examination. (A) Fascicular arrangement of bland spindle cells intermixed with many inflammatory cells (H&E, x40). (B) Spindle cells show abundant cytoplasm and conspicuous nucleoli, admixed with plasma cells and lymphocytes (H&E, x200). Tumor cells express smooth muscle actin (C) and cytoplasmic expression of anaplastic lymphoma kinase (D) on photomicrograph (x 200).
Discussion
IMT is a rare tumor that can occur in various tissues and organs, and is characterized by a mass or nodule made up of spindle-shaped cells called myofibroblasts, along with an inflammatory response. Inflammatory spindle cell lesions in previous researches exhibit a complex nomenclature, which has led to researchers frequently using the terms “IMT” and “inflammatory pseudotumor (IPT)” interchangeably in scientific papers. Recent studies have indicated IMT should be considered a neoplasm that may recur or metastasize [4], and IPT as a heterogeneous non-neoplastic condition characterized by an inflammatory lesion that can mimic a tumor [5, 6]. The exact cause of IMT is not well understood, but it is believed to be related to an abnormal immune response or genetic mutations. Symptoms of IMT can vary depending on the location and the size of the tumors, but they may include pain, swelling, and difficulty breathing or swallowing. Because IMT often mimics malignant neoplasm clinically, radiologically and histopathologically [7, 8], it can be confirmed through pathologic examination with the presence of myofibroblasts. Treatment for IMT may involve surgical removal of the tumor and the prognosis is generally favorable, especially if the tumor is caught early and effectively treated.
Although rare, when IMT involves the gallbladder, it can trigger acute cholecystitis, and if the lesion extends to the bile duct, it can also cause cholangitis, biliary colic, and obstructive jaundice. In our case, the lesion was confined only to the gallbladder without any involvement of the bile duct, and the symptoms were abdominal pain and weight loss.
The radiologic findings of IMTs are nonspecific and can have different radiologic features depending on its location and size [9]. CT and MRI are the imaging techniques of choice. In general, in contrast-enhanced CT scans, IMT may manifest as homogeneous or heterogeneous lesion, exhibiting variable enhancement on delayed acquisitions due to the presence of abundant fibrosis. These observations are consistent with those seen on gadolinium contrast-enhanced MRI. IMT typically exhibits low signal intensity on T1-weighted and T2-weighted images, reflecting the presence of fibrotic tissue [9]. However, it can appear as a mass with intermediate signal intensity on T2-weighted images. Most common radiological presentation is a well-defined, irregular, and solid mass. It is important to note that these imaging findings are not specific to IMT, and other type of tumors or inflammatory conditions may have similar radiologic features. Therefore, it is difficult to differentiate from other types of tumors and inflammatory conditions. Most of the reported primary gallbladder IMT showed gallbladder wall thickening with or without invasion of the liver parenchyma on radiologic examinations and were thus initially misdiagnosed as advanced gallbladder cancer or severe cholecystitis [2, 3, 10, 11].
Histological confirmation is usually critical to proper diagnosis of IMT. IMT is composed of fascicles of bland myofibroblastic cells mixed with a prominent inflammatory infiltrate consisting of lymphocytes, plasma cells, macrophages, and eosinophils. The lack of atypia, hyperchromasia, and abnormal mitotic figures are distinguishing points from malignancy. The spindle cells stain positively for smooth muscle actin and vimentin, but negatively for S100, desmin, CD100, cytokeratin, CD35, and latent membrane protein [2, 12]. In the current World Health Organization (WHO) classification, IMTs are classified as tumors of intermediate grade due to a tendency for local recurrence and its small risk for distant metastasis [4, 13]. Therefore, it should be followed up even after complete surgical removal.
In conclusion, gallbladder IMT is a rare condition that typically presents with nonspecific clinical and radiologic features, often mimicking a malignant neoplasm. It is imperative for the radiologists to be aware of the existence of IMTs, as early recognition can lead to better treatment options and prognosis, distinguishing it from the more ominous malignant neoplasms that it may resemble.
Notes
Grant support
This work was supported by Soonchunhyang University Research Fund.
Disclosure statement
The authors report no conflict of interest.
